Ted Schaeffer is an internationally recognized urologist specializing in prostate cancer and a returning guest on The Drive. In this episode, Ted provides insights into the role testosterone plays, or doesn’t play, in the initiation and progression of prostate cancer. He unpacks the findings and limitations of the recent TRAVERSE trial, exploring the complex relationship between testosterone and prostate cancer. Ted delves into the molecular nature of prostate cancer, explaining the androgen receptor saturation theory and the potential impact of testosterone on cancer growth. He also discusses the use of the Decipher test to predict cancer aggressiveness and guide targeted treatment. Furthermore, Ted shares how he counsels patients regarding testosterone replacement therapy (TRT), including its safe administration in patients with low-grade prostate cancer. Additionally, he highlights advancements in prostate cancer therapies and biomarkers that help develop precise treatment strategies while minimizing the need for broad androgen deprivation therapy.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- Background on the TRAVERSE trial: insights into exogenous testosterone and prostate cancer risk [3:00];
- The androgen receptor saturation theory: how different organs respond to varying levels of testosterone [10:30];
- The relationship between testosterone levels and prostate cancer aggressiveness: how aggressive prostate tumors have lower androgen receptor activity and rely on different growth mechanisms [16:15];
- Using the Decipher score to assess prostate cancer aggressiveness and guide personalized treatment strategies [23:45];
- Considerations for testosterone replacement therapy: how Ted counsels patients, how TRT can be safely administered in patients with low-grade prostate cancer, and more [31:15];
- Advancements in prostate cancer therapies and PSA as a biomarker for precise treatment decisions minimizing the need for broad androgen deprivation therapy [38:30]; and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
Background on the TRAVERSE trial: insights into exogenous testosterone and prostate cancer risk [3:00]
- The TRAVERSE trial was published a year ago, and it set out to answer the question: Does the use of exogenous testosterone increase the risk of ASCVD in men?
- Peter has written about this trial
- We’re not going to go into great detail with respect to its primary outcome of ASCVD
The short answer is it did not increase the risk of ASCVD
- Peter and Ted found themselves discussing a question of prostate cancer
Tell folks a little bit about what we did and didn’t learn with respect to prostate cancer from the TRAVERSE study
- This study looked at men who were hypogonadal, who presented with some degree of symptoms, and then the idea was to replete their testosterone, bring it up to a eugonadal level
- The bump that they had in the TRAVERSE was pretty small, 140 ng/mL, so a tiny bump with bearing in mind about a 60%+ dropout rate at 5 years
- Very few people were actually maintaining the protocols that they originally set out to do at the beginning of the study
- The bump that they had in the TRAVERSE was pretty small, 140 ng/mL, so a tiny bump with bearing in mind about a 60%+ dropout rate at 5 years
- With that in mind, the idea was: does supplementation of someone’s endogenous testosterone with exogenous testosterone increase one’s risk for being diagnosed with prostate cancer, with the implication that this could address 2 potential concerns
- 1 – Exogenous T would fuel the progression of an pre-existing prostate cancer
- 2 – And/or exogenous T would induce a cancer de novo in somebody with a low T state when you bring them into a higher testosterone state
There is a lot of detail about who was enrolled in the study
- Everybody was hypogonadal and the mean PSA for individuals in TRAVERSE in both arms was around 0.9 ng/mL
- So this is a low risk group of men because we know PSA is the main way that we screen for prostate cancer
- In general, the higher one’s PSA, the higher one’s risk would be of being diagnosed with prostate cancer
On average, these are men in their 60s with low testosterone and low PSAs on average ‒ they are a low risk group, and you take them from a hypogonadal to barely eugonadal state
- Ted explains, “The bottom line for the trial in a secondary analysis pre-specified, was that there were no more prostate cancers diagnosed in men on T replacement versus on placebo.”
The total number of prostate cancers in TRAVERSE that were detected was very low
- In a cohort of 5,300+ men, there were 23 total cases of prostate cancer in the TRAVERSE study [12 in the testosterone group and 11 in the placebo group, see the figure below]
- The features of the individuals who had prostate cancer in TRAVERSE were on average higher PSAs than the median
- Again, the median PSA on entry was around 0.9
- Individuals who were diagnosed with prostate cancer had higher median PSAs and had higher shifts in their PSA while in the TRAVERSE trial than those men that did not develop or were not diagnosed with prostate cancer
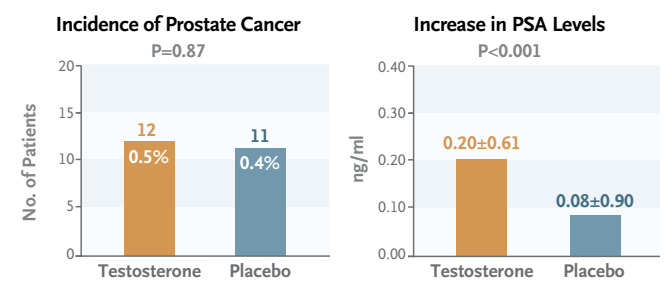
Figure 1. Incidence of prostate cancer in the TRAVERSE trial. Image credit: NEJM 2023
What this study tells us about prostate cancer risk is reassuring in many ways
- 1 – Men with low PSAs have a low risk of being diagnosed with prostate cancer
- 2 – You can use PSA in generally similar fashions when you’re supplementing a man on exogenous testosterone
- That is, you can look at changes in the PSA
- For most men in TRAVERSE, their PSA did not change
- It changed less than half a point over the course of the trial
- And for those individuals whose PSA did go up, those were the men that were at risk for or were subsequently at higher risk for being identified as having or harboring a prostate cancer
There was a figure in the paper that showed the non-statistical significance in the difference between the incidence of prostate cancer in the groups.
- Even though it never comes close to reaching statistical significance (because in large part the sample size is so low), and even if there was a difference, it would be very hard to see
- The incidence curves do diverge a little bit
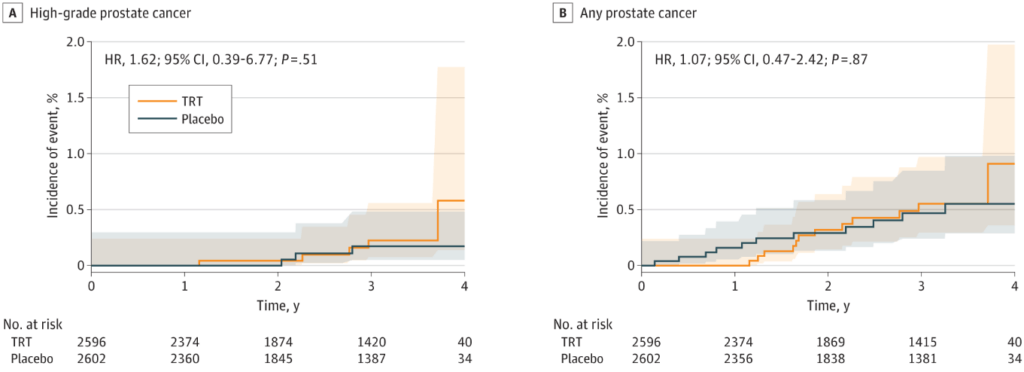
Figure 2. Estimated cumulative indices of prostate cancer in the TRAVERSE trial. Image credit: JAMA 2023
- The study wasn’t long enough or wasn’t large enough to see if this was increasing the incidence or recognition of prostate cancer [the mean duration of follow-up was 33 months]
What are your thoughts on that line of inquiry?
- This is a large cohort [5246 men]
- Ted felt like there is pretty limited data to suggest that levels of testosterone or supplementation of testosterone really are strong and correlated with the induction of or the precipitation of a preexisting prostate cancer
- He personally felt that supplementation of individuals in a hypogonadal state to a eugonadal state is not going to increase their risk for the induction of or the propagation of a pre-existing prostate cancer
In this study, you’re bringing somebody from a state where they have low T to a more eugonadal state, and there’s some interesting work that helps us understand what happens when a prostate grows
- One of the main growth components for a prostate are androgens, either in the form of testosterone or dihydrotestosterone (which has a much higher affinity for the androgen receptor)
- And this really does 2 things:
- 1 – It causes growth and differentiation
- 2 – The sensitivity of prostate cancer cells to these growth hormones (for them androgens or DHT) is different between a cancerous and a non-cancerous cell
- There’s actually much higher densities of androgen receptor within a benign prostatic cell, and therefore they’re much more sensitive to supplementation of testosterone
With that in mind, most of the studies that have looked at supplementation of testosterone in eugonadal men have shown more often than not, that they actually have worsening of their BPH or urinary symptoms
- And that’s thought to be due to the greater sensitivity of benign cells to exogenous T than actually the development or progression of a prostate cancer
- So that’s TRAVERSE plus a couple of other smaller but consistent studies that have been published over the last 2-3 decades within the urology space
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.

Ted Schaeffer, M.D., Ph.D.
Edward (Ted) Schaeffer earned his MD/PhD from the University of Chicago. He completed his internship in general surgery followed by a residency in urology at Johns Hopkins. He is a board certified urologist with an active practice specializing in prostate cancer.
Dr. Schaeffer is Chair of the Department of Urology at Feinberg School of Medicine and Program Director of the Genitourinary Oncology Program at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. His globally recognized prostate cancer research focuses on at-risk populations, diagnosis, treatment outcomes, and the molecular biology of lethal prostate cancer. [Northwestern Medicine]
Website: TedSchaefferMD.com



